'It's made me think that I want to do more now' 💬
— SCIE (@SCIE_socialcare) February 11, 2019
Course delegate Sue Wheatcroft gives her feedback from SCIE co-production bespoke training.
Find out more about the course and enquire: https://t.co/ziGvSFU8Xf pic.twitter.com/8Qc7r4IdBz
Category: Uncategorized
Keynote speech at Comensus Conference (UCLan, 2024)



Speech
Thank you, Mick, and thank you to Comensus, for inviting me here today.
Explain outline of speech (on slide)
Seven years ago, I was sitting in a prison cell, dreaming about what I would do when released. I had a relatively recent diagnosis of borderline personality disorder (BPD) and had quickly learned just how much stigma and misunderstanding surrounds the diagnosis. The judge in my case knew nothing about it and was persuaded by my local community mental health team that it was untreatable and that neither they, nor the probation service, were willing to supervise me. This resulted in me being given a custodial sentence rather than a community or suspended sentence.
I learnt a lot about injustice in prison and how both the mental health and criminal justice systems were failing people, and I wanted to do something about it. I wanted to help people. The thing was, I had no idea how to go about it. Like most people in prison, I knew nothing about experts by experience and how they were working to bring change. As far as we were concerned, no-one cared about us other than our own families and friends.
I have decided to include my prison experience in my speech because health and social care is a vital part of it. Women especially, experience poor physical and mental health and many are living with trauma. I look on this part of my life, and the events leading up to it, as my crisis period. The time since my release I see as my recovery period.
I know there are a lot of people here that are heavily involved in patient and public involvement, and I wouldn’t presume to know more about it than any of you. I want to share my story with you to highlight some of the different opportunities that I found, and also, some of the pitfalls.
So, back to my prison cell . I would start a support group, I thought. Having never attended one myself, I thought they were all run the same, like AA . Hello, my name is Sue and I have borderline personality disorder . Of course, it didn’t turn out like that.
After my release, I was put in contact with someone at Rethink Mental Illness, who helped me to set up the Derbyshire borderline personality disorder support group. It’s now in its seventh year and has helped over 400 people, including several from overseas.
I have always been proud of the group, of course. It provides a space where like-minded people can come together and support each other. But I wanted to do more. I wanted to get involved in bringing change, so that our group will be supplementary to, rather than in place of, adequate treatment.
Through Rethink, I was introduced to Healthwatch, and joined their advisory panel, which was made up of experts by experience. Through my work there, I was put in touch with an agency in London, who were working for prison reform. And through them, I became part of the East Midlands Health & Justice team.
All this happened relatively quickly, but I was enjoying it. I was convinced that I was making a difference, and in some ways, I was. I went into prisons to interview people with cancer on their experiences of treatment. I co-produced and co-delivered a pre-release skills course in a women’s prison and then developed a best practice guide.
I even went back to the prison I was in. I hoped I would see the officers who had, so often, accused me of being an attention-seeker. I wanted to say ‘see, you were wrong about me!’. Unfortunately, or perhaps fortunately , I didn’t see anyone I knew.
I learnt a lot from going into the various prisons. As a prisoner, I could only see one side, which wasn’t always positive. But going in as a researcher, or to deliver a skills course, gave me a different perspective. I saw how overstretched the officers were, as well as the serious lack of communication between each sector of the prison. My colleague and I sat waiting for over an hour for an escort to take us to the interview room because the reception staff were busy and forgot to ask for them.
I thought back to a time I had asked an officer to take me to the visiting room. He said he would send someone to fetch me, but they never turned up and I missed my visit. I took it personally and thought they had done it on purpose. But sitting there waiting for an escort, I could see how easily it could happen.
My biggest achievement at that time, I felt, was being part of the east midlands prison partnership board. It was a partnership between the NHS and the criminal justice system, two organisations I felt passionate about. As a board member, I was able to bring items to the agenda, see them minuted, and then actioned. This was true co-production.
I told the board of my experience in prison after I had fell and dislocated my shoulder. I was left in pain for 5 days before they allowed me to go to hospital to have it corrected.
This kind of lived experience can be particularly useful for those at the top, who are unaware of what goes on a daily basis.
On the board was a prison director, who said that my case must have been an isolated incident. It would never happen in any of his prisons, he said. I suggested, politely, that someone in his position would not necessarily be told of such rudimentary matters.
I knew this director didn’t like someone like me being on the board. Whenever I spoke, he either sighed loudly or looked pointedly at his watch. Fortunately, the Chair of the meetings was the one who had invited me onto the board and made sure I had my say. It was agreed that I, and the rest of the health and justice panel, should carry out research into the subject, and this led to another best practice guide for prisons; this one on escorting prisoners to and from the local general hospital.
At another board meeting, I brought up the issue of physical abuse by officers on prisoners. I told of my own experience of this and was advised by the director to bring an assault charge against the officer. I was surprised at this and thought that maybe I had got the director all wrong. But then he followed it up with, of course that would mean that you wouldn’t be able to carry on with this board because it would be a conflict of interest. I told him that I could do more good by staying on the board, but thanked him for his ‘concern’.
In time, the work I was doing started to affect my mental health. I couldn’t risk another crisis and so decided to take stock of which jobs I enjoyed and which ones I found too stressful. Also, which organisations truly believed in PPI, and which included people with lived experience merely to tick a box to say they did? Was I valued, or was I being used.
Firstly, Healthwatch. Several times they asked me to represent them at multi agency meetings regarding crisis plans, but each time, the police would veto it, saying it was inappropriate because of my criminal record. After a while Healthwatch, understandably perhaps, stopped asking, and so I left.
The agency in London got me involved in several things, which I enjoyed. For example, the cancer in prison project. This had been run jointly by a major cancer charity and a university in the south of England, and it led to me, and the two other lived experience members involved in the project, contributing to a published academic paper.
But then I discovered that the agency had charged the project funders an enormous amount of money just to provide our names. The three of us were paid just £45 per day by the agency and, although I didn’t start this work to make money, I didn’t like the idea that the agency was using me to make money for themselves. So, I left. Around the same time, I left the prison partnership board. I felt that I had gone as far as I could and there were others on the health and justice lived experience panel that could take over.
When I was first asked to get involved in this kind of work, I felt grateful for being asked and vary rarely turned anything down. But I wasn’t always fully prepared. For example, the males I interviewed about their cancer treatment were all sex offenders and were serving long sentences. I went there with the idea that they were human beings, and I had a job to do. But, in subsequent weeks I felt guilty.
I had joked with some of them, mainly as an icebreaker so they would feel comfortable. My colleague and I got the information we needed, but several times we had to stop them from talking about their offences. I ruminated about this for a long time after, the guilt came from the knowledge that I had joked with someone who, if defined by their crimes, were monsters. In a way, I felt like I had let down their victims.
But I learned a lot from that experience. Self-care and self-compassion are vital in this kind of work, whether we interview someone else or share our own stories. If you’re new to PPI, I would advise being selective in what you take on and beware of tokenism & exploitation. Consultation and Informing can be just as valuable as coproduction, but it’s important to recognise what you are contributing. Organisations should not use you to tick the co-production box if that’s not what’s happening. Honesty, trust and transparency are vital. Equally important – you should be enjoying what you do.
As you will know, much of PPI work is voluntary. Payment can be a contentious subject, but I think it’s a matter of personal choice. I was recently asked by my local police to do a training session on personality disorders for some of their 999 call handlers. I was interested, of course, and would have done it for free. But then I was told that, although it’s usual to provide payment for this kind of work, as they do with the carer’s association, the hearing and sight impaired, and the various other organisations they invite, they could not pay me because there was no budget for personality disorders. I felt insulted on behalf of my community. Why were we being treated differently? So, I regrettably declined, but said that I would make myself available as soon as the budget allowed for it.
After giving up so much of my work, I had more time to concentrate on my writing. I was, and still am, an academic. Before prison, I was a historian and wrote a book about disabled children during the second world war. But after my crisis period, my work became all about prison reform and mental health. I had several articles published, including one in Custodial Review, a magazine for the police and prison services.
I decided to write an article for an online journal meant for probation practitioners and researchers. I wrote about the importance of boundaries in the probation officer and client relationship, and it was published in 2021. As an introduction to the article, the editor wrote,
In this issue, we have a challenging article from a service user, Sue W. It does not make for comfortable reading but Sue’s analysis of what could and should have been done differently in her supervision – not only by probation but also by community mental health services – is eloquent, and she argues that achieving the right balance between empathy and professional distance requires a sophisticated level of skill and awareness.
I was proud of the article and pleased with how it had been received by the editor. But a couple of weeks after its publication, a colleague told me they couldn’t find it. The journal was online but without my article. Fortunately, I had downloaded the issue as soon as it had been published so I compared that with what was online now. They were the same in every way, except that my article had been withdrawn. I phoned the editor but was told she didn’t want to speak to me.
To this day, I don’t know why that happened, but it had an enormous effect on me at the time. Fortunately, since leaving prison I have been seeing a private therapist and so was able to discuss it with her. She helped me to move on from it and advised me to stick to the voluntary sector for a while. I wrote a few blogs and participated in health and justice panels, podcasts and webinars. And I became a reviewer for Research Involvement and Engagement, a coproduced journal, which focuses on patient involvement and engagement in all stages of health and social care research.
Then, in July 2022, I delivered a speech at Rethink’s 50th anniversary event held at the Houses of Parliament. The event was attended by Gillian Keegan, who at the time was the Minister for Mental Health and Social Care. She listened to my speech, was polite and encouraging and said that yes, things had to change. She wanted to get involved, she said, but I was sceptical, and rightly so. Two months later she moved into a new post, and we never heard from her again.
I decided to try a different way of raising awareness. Every single day of my time in prison I had written something about prison life. What I saw and how I felt. I talked about other prisoners, the officers, healthcare (which was run by the NHS rather than by the prison) and the prison system itself. How it worked on a daily basis. I had kept everything and now thought it was time to turn it into a book, which I published on Amazon at the beginning of 2023. After that, I wrote about the health and justice system from my perspective, using my case as an example, and I published that at the end of 2023.
Looking back at the work I have done, a lot of it has been by consultation and sharing information, as well as co-production. Here’s a few more examples…
Slides
Conclusion
For those of you who are here today from organisations that already include people with lived experience, or are thinking of doing so, please value them. Their insight is extremely important in making services successful. And please look after them. This kind of work can be enormously helpful to someone who is trying to make sense of their own experiences, but it can also be stressful and exhausting.
Like most people working in PPI, I am passionate about the work I do. It’s helped enormously with my recovery, and I have learnt a lot. And I think I have managed to find the right balance in order to stay psychologically safe. I’ve learnt what my limitations are, the importance of self-compassion and of showing compassion to others, and to try and see both sides of an issue.
But we’re always learning, aren’t we? And I’m looking forward to learning about other people’s experiences and different methods and experiences of PPI at this conference. There are some great speakers lined up, so I hope you all enjoy it as much as I know I will.
Thank you!
Webinars & Videos & Podcasts
Home
Contents
- Charing Rethink webinar
- Video talking about a coproduction training session
- Video with Farah Damji
- Panel appearance at the Fair Access to Justice event in Canterbury
- Webinar presentation for Fair Access to Justice
- Co-chairing the Innovation Insights webinar
- Podcast: Rebel Justice
- Revolving Doors Podcast: Childhood Adversity and Multiple Disadvantage
- Criminal Justice video
ONE
TWO
Go to: https://twitter.com/i/status/1094914520982654976 for Sue talking about a training session on Co-production
THREE
FOUR
FIVE
SIX
SEVEN
Podcast: Rebel Justice Two (2022)
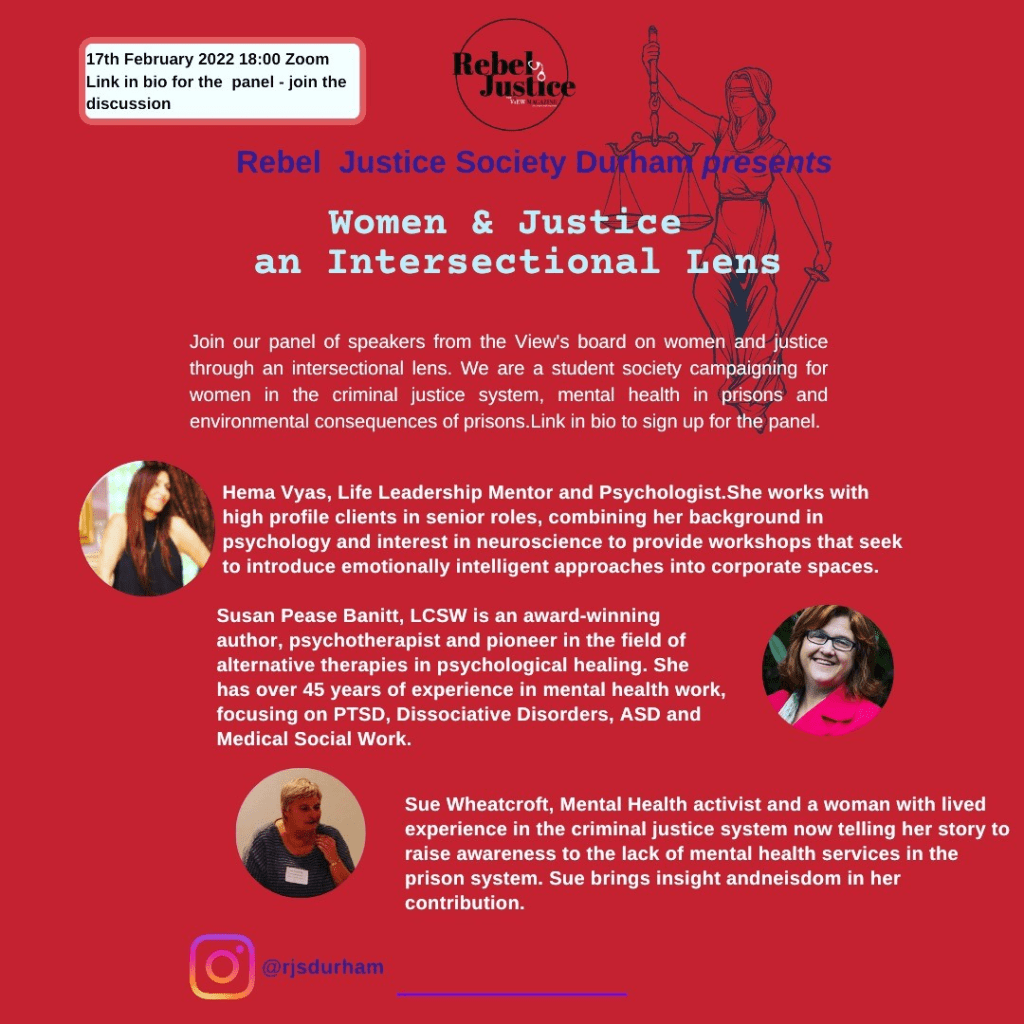
Schedule
Narince Erkan introduces the Durham Rebel Justice Society and the session’s theme of viewing women and justice through an intersectional lens.
Hema Vyas introduces herself and Omnipreneurial Psychology, which explores how we can do business in a way that takes care of people and the planet through heart-centred therapy.
Hema Vyas speaks about how women in prison are a mirror for the rest of society. Qe as a society are failing to address why prisons aren’t working, instead of giving compassion to nurture transformation.
Sue Wheatcroft introduces herself and speaks of her experience of mental illness, how this led her to prison, and the culture of bullying and harassment of women by officers in prison.
The View’s film about Annelise Sanderson, an 18-year old girl who died in custody at HMP Styall.
Amanda Hawick introduces herself and gives insight into her role as an Independent Prison Monitor of in Scotland. This Scottish system helps ensure that prisoners’ human rights are upheld and that life in prison contributes to their rehabilitation.
Susan Pease Banitt introduces herself and explores the urgent need for trauma-informed care in prisons. She advocates for prisons to align with the prescriptions of neuroscience to help people recover and become more functional.
Susan Pease Banitt leads a meditation session, which can be used by women in prison to self-regulate their nervous systems.
link to podcast:
https://rebeljustice.buzzsprout.com/1893705/10128551
Eight
Revolving Doors Podcast: Childhood Adversity and Multiple Disadvantage (2021)
Nine
Criminal Justice video (2025)
Awards
Home
- Janey Antoniou award (2019)
- Group of the year award (2023)
- University of Lancashire team award (2025)
1. Janey Antoniou Award 2019
Meet Sue Wheatcroft, winner of the 2019 Janey Antoniou Award.
09 November 2019
Today, Saturday 9 October, we are pleased to announce Sue Wheatcroft as the winner of our 2019 Janey Antoniou award for 2019. Sue is a campaigner and group coordinator who lives with Borderline Personality Disorder (BPD). She has made a huge difference on both a local and national level and the judges felt she exemplified what the Janey award is about – challenging stigma and creating change for people living with mental illness. We sat down with Sue to ask her more about her vital work.
What has your experience of the mental health system been like?
When I was in crisis, I asked my GP if I could increase my anti-depressants. He said I was already on the maximum dose and should think about talking therapy. I was referred to Talking Mental Health (IAPT), who said they couldn’t help. They referred me to secondary care, who gave me an assessment. I was then referred to a psychiatrist, who said he would put me on a waiting list for a psychologist and a CPN. I saw the psychiatrist three times within the next twelve months and each time he assured me I was still on the list. Eventually, I phoned the CMHT myself and was informed that I was not, and never had been, on any waiting list. From then on, my mental health worsened, and I offended. I spent 18 months in prison, during which time my (disabled) partner was forced into a nursing home. When it was all over, my partner (now wife) went home together. We have just celebrated 34 years together. We re-mortgaged the house so that I could have private therapy and I am now in recovery.
How did you start campaigning on mental health?
There are currently no dedicated mental health services for personality disorders (PDs) in Derbyshire. This means that, if someone presents to their GP with a PD, they are often told that nothing can be done because ‘there is no PD pathway in Derbyshire’. If they are lucky enough to be referred to an IAPT, they are often turned away because of the stigma of their condition. If they make it to the allowed six sessions and it turns out that it is not suitable, they can be discharged from the whole service for ‘not engaging’. It is common for an individual to be told that they are too complex for a service, or not complex enough. Inevitably, they lose faith in the system. Self-harm and suicidal ideation are common. One in ten people with BPD end their own life and seven in ten make a serious attempt.
What led you to setting up the BPD support group?
When I left prison, I re-mortgaged my house to pay for private therapy. I have been seeing the therapist every week since (it will be three years in February). For some of that time, I received a Personal Health Budget. Even so, I have spent an enormous amount on therapy, but it has been worth every penny. Without it, I know I would not have been able to carry on. However, I realise that not everyone can afford it, and, in the absence of statutory services, there is absolutely no help for people with a PD. There are many PDs, but I only have experience of BPD. The thought of others going through the same experiences as me, makes me feel physically ill. I set up the support groups to help ensure this doesn’t happen.
What was one of your proudest moments when campaigning on mental health…
…was when I first read out my story ‘First Night’ at a conference on ‘Commissioning Together’, organised by Health and Justice and attended by Lord Bradley (author of the Bradley Report). The positive reaction it elicited made me realise how much could be achieved by sharing lived experience. The story was about the shock, guilt, vulnerability and sense of desperation I experienced on my first night in prison. I realised then that it was a way of getting the consequences of inadequate mental health services known to a wider audience than just my home county. This does not retract from the fact that I take ‘ownership’ of my offences.
My most memorable moment is 200 members of the Independent Prison Board singing happy birthday to me after I had given a speech about BPD at a conference in Telford.
My proudest moments relating to the BPD support groups occur every time I witness the support, they give to each other. This can be at a meeting or on the group’s WhatsApp page.
How would you like to see care for BPD change?
I believe that the majority of people, once they have come to terms with their diagnosis, realise that not much can be done for them when in crisis. Two solutions have been suggested by the members. The first is to have a safe place to where they can be taken, voluntarily, to calm down. This could be some kind of crisis centre offering a few hours, or perhaps one or two days, away from the environment in which they reached crisis point. Once there, and this is also the second solution, they should be able to speak to someone who understands; is not judgemental; and has compassion. BPD is highly stigmatised, and individuals are often being accused of attention-seeking, manipulative and acting like a child. This last point is particularly interesting as most would agree that they display childish tantrums. They don’t want to; they can’t help it and are usually ashamed and embarrassed afterwards. Some professionals believe that people with BPD retain the emotional age at which they suffered childhood trauma. Someone can have the mind, body and intellect of an adult but the emotions of, say, a seven-year-old.
Before reaching crisis, and as an attempt to avert it, it is vital that the stigma surrounding BPD, and other PDs, is addressed. I would like to see zero tolerance on derogatory language (attention-seeker, for example). This should be made clear when receiving education and training on personality disorders which, at the moment, is woefully inadequate. Such courses should be made available to all health and justice professionals. This would include psychiatrists and psychologists, as they are often the instigators of stigmatising behaviour. It should also include police, probation and prison officers. People with PDs often end up in the Criminal Justice System. Seventy per-cent of people in prison have a personality disorder. BPD is the most common PD among women in prison.
Derbyshire NHS Trust say they will put more money into talking therapies. This is useless to those with a PD if they are excluded from the service in the first place, or if it is unsuitable for them. This is why we need a pathway (most other counties have one). All training should include facilitators who have lived experience.
It is important that you are passionate about the cause for which you are campaigning. It will be hard work and the sense of responsibility can give you sleepless nights sometimes, but every success, however small, can give you the greatest feeling in the world.
Sue WheatcroftJaney Antoniou winner 2019
How did it feel to win the Janey award?
I received the email whilst at the Supreme Court, where I had given a speech on the stigma of BPD. I wanted to shout it out to everyone but someone else was speaking and I had to be quiet. Also, I knew I had to be careful who I told so that it wasn’t put on social media. I couldn’t wait to get home to tell my wife, Vicky. She talked about putting it in the local paper as soon as I had the award so that everyone will know. Once I had calmed down, I realised how it could help to raise the profile and awareness of BPD, not just in Derbyshire but nationally. I feel very proud but also grateful, to the voting panel, Rethink, the group members and the many organisations and individuals who have given me a chance to campaign.
What would you say to people who would like to start campaigning on mental health, but don’t know where to start?
It is important that you are passionate about the cause for which you are campaigning. It will be hard work and the sense of responsibility can give you sleepless nights sometimes, but every success, however small, can give you the greatest feeling in the world. On a practical level, Rethink Mental Illness is well-equipped to help with such things as the Constitution; Insurance; Code of Conduct; risk-assessment for the venue; DBS checks for co-ordinators; and the other seemingly tiresome but vitally important aspects of setting up a support group. They can also help with promotion, such as leaflet distribution, and will offer continuing support.
If you are unsure about taking such a large step straight away, have a look at the Rethink Mental Illness website for other groups you could attend to find out more about how it is done. Bear in mind that a niche group, such as BPD, will probably be a slow-burner and it’s important that you don’t get despondent. On the other hand, a general mental health support group could take off straight away and you must be prepared, so that you don’t get overwhelmed.
Janey Antoniou was a dear friend of Rethink Mental Illness and an inspirational colleague. During her 15 year career in mental health she worked tirelessly to improve the care of people living with mental health problems. Throughout all her achievements she lived with debilitating depression, anxiety and schizophrenia. The Janey Antoniou Awards recognise campaigners with lived experience who have made a difference to the lives of people living with mental illness through raising awareness, combating stigma and campaigning for better care.
2. Group of the Year Winner 2023
Meet Derbyshire BPD Support Group, our 2023 Group of the Year winner (rethink.org)

After coming out of a four-year crisis, Sue wished there was a specialised BPD support group she could have been a part of. She’d attended more general mental health groups before but didn’t feel these were focused enough on her diagnosis. She created the Derbyshire Borderline Personality Disorder group in 2017, with wishes that nobody else would have to go through what she went through. Sue believes that her mental health crisis was exacerbated by the lack of support.
By the time Covid-19 came around the group had established four venues, but these had to shut because of the pandemic. Instead, the group went online via Zoom. The use of Zoom enabled the group to hugely expand with over 350 users, 13 of which were overseas. The group develops and progresses organically to meet people’s different needs; for example, the group stayed online but smaller and more local in-person events were set up, such as coffee mornings and activities like bowling (funded by external givers).
The group encourages members to create their own networks and Sue hopes that the group is just the start of smaller networks that develop and grow within themselves. It also offers information about themselves, referral advice, what the statutory services can offer and a quarterly newsletter. This newsletter allows people to contribute and share their own stories, share creative work such as art and poetry, features advice articles and articles about famous people living with BPD, as well as any new information or research. The group also has crisis cards for its users, designed for instances when they may get picked up by the police, paramedics etc, to explain that this individual is in a crisis and is not a criminal. Sue has also set up an Attachment Group which is run via email. Attachment is a huge part of living with BPD so the group offers exercises on dealing with attachment.
As well as this, a key part of the development of the group has been creating WhatsApp groups for specific needs. Six of these WhatsApp groups have now been established:
- General group chat. This has around 100 members.
- Positivity group. Sue understands that with mental illness comes its negative reality. No negative text is allowed in this chat to give people a positive boost for their day.
- Men with BPD.
- Parents with BPD.
- Virtual Walking Group where people send in pictures of their walks, such as canals or woodland, to then encourage people to get out into the fresh air.
- Parent and Carer Group.
3. University of Lancashire team award (2025)
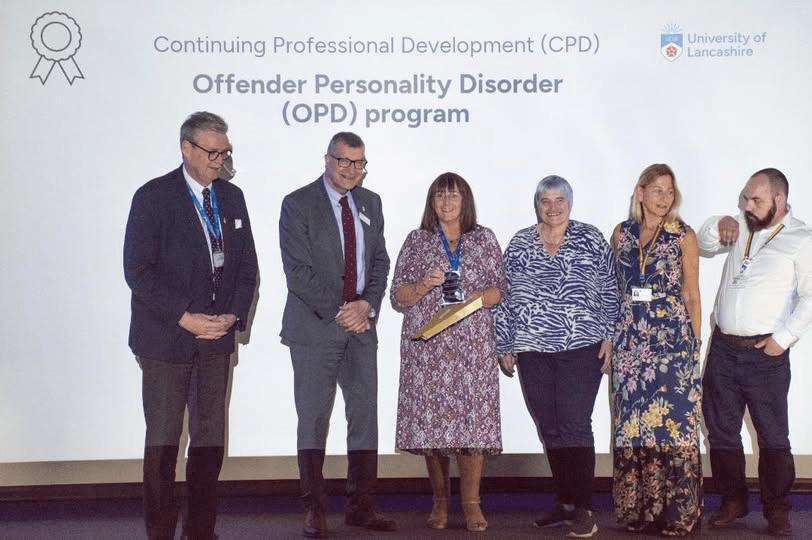
A pedagogic evaluation comparing face to face and online formats of a multi-professional offender personality disorder (OPD) higher education training programme (2023)
Gary Lamph, Alison Elliott, Sue Wheatcroft, Gillian Rayner, Kathryn Gardner, Michael Haslam, Emma Jones, Mick McKeown, Jane Gibbon, Nicola Graham-Kevan, Karen Wright
The Journal of Forensic Practice
ISSN: 2050-8794
Article publication date: 27 September 2023
BLAME: a personal account of the UK Health and Justice system
Out soon!
Revolving Doors Podcast: Childhood Adversity and Multiple Disadvantage (2021)
COVID-19 stories
Home
- BPD, COVID-19 and Me
- Experts by experience: the effects of isolation during COVID-19 pandemic
1. BPD, COVID-19 and Me
Published in RETHINK
https://www.rethink.org/news-and-stories/blogs/2020/08/bpd-covid-19-and-me/
Sue Wheatcroft is a campaigner and group coordinator who lives with Borderline Personality Disorder (BPD). Winner of our prestigious Janey Antoniou award in 2019, she’s made huge inroads in challenging stigma and creating change for people living with mental illness. In this blog, she explains what it is like living with BPD, and what impact the Covid-19 pandemic can have on the way we all look at the condition.
With so many deaths, and key workers putting their lives at risk, I feel a little self-indulgent talking about my problems, but everything is relative, right? I am a full-time carer for my wife; I also have a diagnosis of Borderline Personality Disorder (BPD). Some of you will have a good insight of what this is, others will have never heard of it and, rather worryingly, some people will only know the negative aspects of the condition and believe the hype and stigma caused by misunderstanding, fear and ignorance.
This is not the place to discuss BPD in detail; it’s a big subject and deserves greater time. What I can say is that we who have the condition, struggle to manage our emotions. ‘We all do, sometimes’, you may think, but how many of you go from passive to aggressive at the flick of a switch? A seemingly innocuous comment from someone we care about can be misinterpreted or exaggerated, bringing about an immediate wish to die. It is extreme and it is serious. One in ten people with BPD end their own lives.
- We who have the condition, struggle to manage our emotions. ‘We all do, sometimes’, you may think, but how many of you go from passive to aggressive at the flick of a switch?
There are many studies currently being carried out on the societal effects of the Coronavirus outbreak, and what it could mean for us all moving forward. There is a lot of things that need to be considered within that: domestic abuse & homelessness among other things. These are not new problems!
The issue that has come to the fore more prominently, is mental health. Over the past few years, depression has received increasing attention although, sadly, not so much the less common issues, such as BPD. Hopefully, that is about to change. It is expected by many, that the heroic actions by health professionals, and others, in caring for the more serious COVID-19 patients, will result in an increase in cases of PTSD. Both BPD and PTSD are trauma related conditions and BPD is known by many as Complex-PTSD. Undoubtedly, there will be help for COVID-19 heroes if they need it, and rightly so. Hopefully, if we manage to raise awareness and understanding of BPD, some of that help might trickle down to those with the condition.
- The reason I am writing this, is because it is time for people with BPD to get the help they need.
The reason I am writing this, is because it is time for people with BPD to get the help they need. I run support groups for those with the condition, and their families and support workers. There is a serious lack of statutory help and the little there is, has been put on hold due to COVID-19. Now, with the lockdown and social distancing measures, these support groups have also been put on hold, leaving people alone with their difficulties. Not everyone can discuss their feelings on zoom! For anyone who thinks that BPD is ‘just bad behaviour’, imagine the following scenario:
Female, aged 7, subjected to physical, sexual, and emotional abuse by father, and abandoned periodically by mother. Aged 14-16, runs away, police take her back, telling her she is a nuisance; takes overdose, spends several days in A&E, told she is a bad person for worrying her parents; bullied at regular school for having nervous tics; attends special school but is still bullied; admitted to psychiatric ward but is traumatised by seeing an elderly man being aggressively forced-fed by two male nurses; aged 16, discharged from adolescent mental health services. Leaves home with violent boyfriend…
This is not an isolated case, by any means, but should people like this be blamed for developing BPD… for struggling with their emotions and all the other distressing effects of the condition? Can you see the similarities between this and PTSD? Isn’t it time to stop the stigma of BPD and introduce a little compassion? If you are a health worker, prison officer, police officer or probation officer, please take some time to understand this condition. Seventy per-cent of people in prison have some form of personality disorder and BPD is the most prevalent among women. I know from experience, that this is an avoidable outcome, but without a better understanding and more help, it will not change.
Both Rethink Mental Illness and Mind have produced very good information booklets on BPD. If you would like to know more about our support groups, please contact me at derbyshireborderlinepd@gmail.com
2. Experts by experience: the effects of isolation during COVID-19 pandemic
Article: Experts by experience: the effects of isolation during COVID-19 pandemic • WEPHREN
It has been said that self-isolation due to the threat of Coronavirus is ‘just like being in prison’. As someone who has experienced both, I feel well-placed to say that, although there are certain similarities, it is not the same!
Let’s ignore the fact that prisoners are currently experiencing their own lockdown, being confined to their cell 23 hours per day, with only one hour to shower and exercise. When people say it’s like being in prison, they most likely mean prison on a ‘normal’ day, i.e., before the advent of the Coronavirus.
One of the main issues of isolation, whether in prison or in one’s own home, is boredom. Those in prison who still have their privileges (any ‘bad’ behaviour can lead to a loss of these) will have a TV in their cell, and books from the library or sent in by friends/family. Many prison wings have a snooker table. Most prisoners have a job or education classes to keep themselves busy four and a half days a week, and there is a gym. Largely due to bad press, prisons are seen as easy, but think about the monotony of having this small set of activities, every week, month or perhaps even years, broken up only by medical appointments and the occasional visit. Then add to this the fact that staff shortages often lead to more in-cell time than is recommended or even humane!
Those on lockdown in the community may also become bored, depending on their particular circumstances. For example, most will be with their own family; those who can afford it are able to order in items to keep themselves busy; they will have no restrictions on online activities, and the hour of exercise can take place in a different area (close to home) each day – as opposed to the same prison exercise yard.
Another problem of isolation is loneliness, although this is not so straight forward. People in prison can be lonely because they have very little contact with their friends and loved ones. Those who do not make friends easily will feel this loneliness even more. For others, prison offers a community spirit that many prisoners crave. They may become institutionalised and, if they do not have a healthy support system in the community, they expect to, and do, return to prison soon after release.
Loneliness in the community, again, tends to depend largely on the individuals’ situation before the lockdown. Those who lived with others continue to do so. Although they may miss certain people, they are not totally alone (although it is possible to be lonely in a crowd if there is no personal connection). However, for those who lived alone and continue to do so, the loneliness may have worsened, especially if they previously had the occasional visit from friends, family members, support workers etc.
The issue that is most common to both people in prison and under community lockdown, is fear and anxiety. In prison, people can live in fear of other prisoners, prison officers, their potential sentence (if on remand) and their physical and mental health. For these people, the sense of being alone, without easy access to information and support, will make that fear/anxiety more extreme.
Those self-isolating in the community due to the Coronavirus will, naturally, be in fear for their own health and that of others. They may even be in fear of loss of life. However, although this fear might be stronger than that felt by prisoners (in a non-Coronavirus environment), there is more access to information and support in the community. In addition, contact with loved ones outside the home, whether by phone or social media, may act as a source of comfort.
All these issues: boredom, loneliness, fear and anxiety, are detrimental to an individual’s mental health. The vast majority of people in prison have some kind of mental health problem which is, more often than not, exacerbated by the stresses of living in prison. Although not as prevalent in the community, most individuals with mental illness whether in prison or community, have suffered from the lack of services caused by under-funding and, to some extent, by a certain amount of apathy and/or stigma among commissioners and the general public.
Regardless of whether self-isolation due to the coronavirus is ‘the same as being in prison’, if the general public think it is, then it may have a positive effect on prison welfare. To some extent, public opinion dictates government policy and it is thought by many that prisoners have a ‘cushy’ life, rather than suffering for their crimes. In law, punishment should be the separation from the rest of society, and not the conditions under which they are made to live. With this in mind, members of the public might realise just how ‘punishing’ it is to be kept away from loved ones; knowing that you cannot be there for them if they need you; the distressing effect of no physical contact with, say, children and/or grandchildren; fear of what could happen next; and the uncertainty of whether life will ever be ‘normal’ again.
The circumstances in which we find ourselves at the moment are unprecedented but appear to have brought out the best in people. Life has slowed down considerably, giving them time to re-evaluate what is important. Perhaps this can be capitalised upon when reviewing prison reform.
Sue Wheatcroft is Expert by Experience at Revolving Doors Agency in England (LINK http://www.revolving-doors.org.uk/). She is also a Research Assistant in the national Cancer Care in Prison Study (How is cancer care best provided to patients in English prisons? Assessing the disease burden in the prison population, experiences of diagnosis, treatment and support, and of receiving and providing cancer care LINK: https://www.journalslibrary.nihr.ac.uk/programmes/hsdr/165253/#/)
Dying on the inside: Britain’s ageing prisoner problem
With more than triple the number of prisoners aged 60 and over today than there were 15 years ago, the strain of caring for them is having detrimental effects on their health… and the system. Emily Goddard reports
Bolted gates, closed doors and impenetrable barriers – of both the physical and symbolic kind – are intrinsic of the prison estate. Yet the door of a room on the healthcare wing of a category B prison remains conspicuously open. Inside lies a man in his eighties, unable to get out of bed and constantly watched by nurses, both day and night, because the end of his life is near.
“The Prison Service is paying for an outside carer to come in to look after him,” says Michael, a prison officer who works at the prison and does not want his real name to be used. “He’s got to the age where he just can’t do anything. He doesn’t leave his room, his dinner has to be brought to him every day, if the carer is not there the nurses have to get him out of bed and put him on the toilet. He’s reaching the point where he could go any day.”
By Michael’s estimation, half of the people in the prison where he has worked for five years are beyond the age of 45. And the dying octogenarian is by no means the oldest man there: Michael works on a wing where a high-needs 94-year-old is housed in a specially adapted disabled cell.
“He isn’t able-bodied,” the prison officer says. “He has to walk with a Zimmer frame. And I think he’s got Alzheimer’s because he forgets to use it and is constantly falling over. We have to go into his cell to pick him up and call the nursing staff.”
Care for elderly prisoners ‘inconsistent and only set to get worse’
Michael describes various times when he has caught the prisoner attempting to walk outside his cell without his frame; it bears a startling likeness to the everyday happenings in a care home environment. “I’ll notice and then have to support him to walk to the medication hatch. Then I’ll have to support him back and remind him to sit down because he gets out of breath very easily. I’ll tell him to stay there and I’ll go to get his food from the servery for him.”
Then there are the frequent visits to hospital that require at least two officers, plus a third tasked with driving, to take the nonagenarian and other elderly or unwell prisoners to routine medical appointments. “This is detrimental to the staffing levels in the establishment. We need as many boots on the ground as possible,” Michael says.
Those boots on the ground are increasingly finding themselves supporting an ageing prison population. The oldest person in prison in England and Wales has a whole decade on the oldest man in Michael’s prison. Ralph Clarke is a 104-year-old great-grandfather jailed for 13 years in 2016 for historical sex offences dating back to the 1970s and ’80s.
People aged 60 and over are the fasting growing age group in prisons in England and Wales – there’s more than triple the number inside today than there was 15 years ago. Almost a fifth of the more than 82,000 people serving sentences across the prison estate in England and Wales are now beyond the age of 50. More than 1,800 of them are 70 or older and, among that number, more than 300 are over 80.
Michael says the surge in older people entering prison has been noticeable. “We’re used to getting the young lads that are messing about on the street,” he says. “We get between 20 and 30 [people coming into custody] a day and recently there’s not so many 20 to 30-year-olds, it’s more 40 to 60-year-olds.” The reason for the trend, he suspects, is partly down to rising numbers of people coming forward to report historical sex offences in the wake of high-profile cases involving household names.
The way I look at it is if one of my relatives, one of my friends were to end up in prison, how would I want them to be treated. I always try to replicate that in the way I deal with people. Everyone is just one mistake away from being there, one mistake away from a custodial sentence
William, not his real name, is a fellow prison officer working in another category B prison in England. He has seen a similar influx of older prisoners and agrees with Michael on a possible cause. “Operation Yewtree, Jimmy Savile, all these other big media events have seen an awful lot of people come forward to say: ‘It [sexual abuse] happened to me,’” he explains. “So although you’ve seen the likes of celebrities being locked up for it, what hasn’t been so widely publicised is that there’s a lot of what I’d call normal people who have been locked up for sex offences too. If the abuse happened in the Sixties and Seventies, by definition, those blokes are now in their sixties, seventies and eighties.”
Although the rising number of older people entering the prison he works at is evident, William suggests it is far more pronounced in other places. He says he has friends who work as prison officers at HMP The Verne on the Isle of Portland in Dorset. This is a specialist category C prison for men convicted of sexual offences – where Gary Glitter is rumoured to be among the almost 600 men held there. Of the prison, he says: “If you were to take a walk around there, it would look like a very secure old age people’s home.”
The prison officers’ evaluations are borne out in data that reveals almost half (45 per cent) of the over-fifties in prison have been convicted of sex offences. For those aged 80 and older, that figure jumps to 87 per cent. Michael says, however, he has seen older people being brought in for stealing food – “because they simply couldn’t afford to buy it”.
Just as the ageing population beyond the bounds of prison walls is more likely to have complex health problems than its younger counterpart, older prisoners typically have extra physiological and psychological needs. “A lot of them we have to locate flat (provide ground floor accommodation) due to mobility issues, they might walk with a stick or a frame or crutches, you can’t put them upstairs. That puts pressure on the prison and the estate a whole,” William explains.
John is 54 and spent three months in prison before being released in May 2018. He has mobility problems and has pins running up his right leg after being involved in a motorcycle accident many years ago. When he was taken into custody he was put on the top bunk of a bed. “I was trying to clamber up,” he says. “This went on for about a week and I got pretty ill, but in the end they did give me a big cell on the ground floor.”
Meanwhile, Sue, who is 59 and went to prison for the first time in 2015 before being released in February 2017, says fellow prisoners rather than staff often managed intimate elderly care. Although she was serving a short sentence, Sue was put on a lifer’s wing – as well as in segregation for five months because of mental health problems – alongside women in their seventies and remembers older people “sticking together”. “They were grateful for just being all together,” she says.
“If someone was incontinent it would be another prisoner, a friend on the wing, who would help her, the help wouldn’t come from the officers,” Sue continues. “They would get them the sanitary wear but as far as anything else goes it’s down to the people you’re with on the wing. It’s better to have friends do it, but there is the guilt of asking them all the time and you can’t expect that. It depends on how severe your problem is. If you’re really incontinent you can’t expect anyone to do that all the time.”
The MoJ says it is helping prisoners learn how to support those with lower level social care needs in the same way family or friends may do with those living in the community.
William has seen this coming together of older prisoners to support each other too. In his previous job in a category C jail where several prisoners used wheelchairs, one prisoner became a wheelchair orderly, playing a similar role to that of a porter in hospital. “He is essentially a taxi service,” William explains. “You call his residential unit and say I need a wheelchair from wherever the prisoner is to wherever they’re going and he’ll be on his way.”
Aside from the practicalities of housing older people in overcrowded and sometimes poorly equipped prisons, there are the regular hospital visits and inpatient stays on wards. Just the day before we speak, William had been sat for 12 hours at the hospital bedside of a prisoner in his eighties who has cancer and was jailed for almost six years in November 2019. The man has been in hospital since before Christmas and each bed watch shift requires two prison officers. “Almost continuously for the last year we’ve had an old prisoner in hospital,” William says.
But not all hospital appointments go ahead as planned. The Prison Reform Trust says it continues to hear of people facing challenges when trying to access healthcare, including mental health services – and the consequences can be severe. The charity makes clear that the blame does not always lie with the healthcare service itself and is calling for a national strategy with estate-wide input to remedy the situation.
“We regularly hear about external hospital appointments being cancelled due to lack of staff or transportation – delaying diagnosis and disrupting routine and urgent treatments, and causing a great deal of stress to patients,” a spokesperson says. “For the health needs of older prisoners to be met, both healthcare services and prison operations must be tailored to the population profiles and projected need of each prison.”
Tony, who has served several sentences in multiple prisons, echoes the Prison Reform Trust’s concerns about the outcomes for unwell older prisoners. He was released for the last time – last, because he did “a lot of hard work” to ensure everything is behind him now – in November 2018 at the age of 53 and has older friends in prison who have cancer. He believes “100 per cent they would stand a better chance if they could’ve got to [hospital] appointments regularly”. He adds: “The negative impact on their illness gets magnified. It definitely gets made worse.”
A freedom of information request to HM Prison Service asking for the number of outpatient hospital appointments cancelled for prisoners revealed the Ministry of Justice could not answer my question because it does not hold the information. “This is because there is no legal or business requirement for the MoJ to do so,” the response reads.
The MoJ says every effort is made to ensure inmates get to necessary external appointments and that its capacity to escort prisoners has been enhanced by the recruitment of 4,400 prison officers since 2016. William admits, however, that despite trying to avoid them, appointment cancellations do happen.
Christina Marriott, the chief executive of Revolving Doors Agency, is alarmed by the impact barriers to healthcare can have on people in prison and highlights the fact that the damage can be felt even after they have been released. “Of course, prisons don’t set out to make you less healthy, but conditions in prisons and poor facilities can make your health go from bad to worse,” she says. “If people don’t get the healthcare they need, it costs lives. Since 2011, the number of people who die after being released from prison has increased fivefold. That’s a staggering and depressing fact. Meeting health needs head on and early on is the smart thing to do, it saves lives and it has the power to change them.”
While positive change is theoretically one of the key principles underpinning rehabilitation of people who have committed crime, there are concerns that little progress is being made to facilitate that for older prisoners. The Prison Reform Trust says it is not convinced that Her Majesty’s Prison and Probation Service (HMPPS) is fulfilling its duties under the Equality or Human Rights Acts in relation to older prisoners. And there is unequal access, the charity says, to the full rehabilitative benefits of prison.
For the health needs of older prisoners to be met, both healthcare services and prison operations must be tailored to the population profiles and projected need of each prison.
That notion becomes yet more troubling when recent changes that could potentially see the prison population ageing still further are considered. Several factors are at play: there is an increasing tendency for judges to hand down tougher sentences – almost half were longer than four years in 2019, compared with a third in 2010; and the automatic halfway release for some serious offenders will end from April under legislation brought in at the beginning of 2020 that will see the release point change to two-thirds of the way through sentences.
The government believes, however, that the prison population is unlikely to grow older – quite the opposite. The MoJ’s most recent prison population projections predict a decrease in over-fifties between 2019 and 2024, while the number of over 60 and over 70-year-olds is forecast to remain constant. That report was published before the policy changes were announced in January and makes clear that it does not take them into account.
The Prison Reform Trust expects most people would view the projections “as optimistic at best, and at worst bearing little relevance to the new reality”, particularly in light of the government’s criminal justice system overhaul. “More police officers to investigate crime; more prosecutors to charge; and more draconian sentencing legislation all point to an increase in demand for prison places in the medium term,” a spokesperson says.
People already in jails getting older and longer sentences are not the only factors contributing to the ageing prison population. There has also been a marked rise in the number of over-seventies being sentenced to immediate custody at courts in England and Wales in the past decade.
Figures obtained by The Independent reveal an 85 per cent increase in men aged 70-plus entering custody directly from courts between 2010 and 2018 (253 individuals to 470). For women, who make up only about five per cent of the overall prison population, there was a staggering 450 per cent surge (from just four in 2010 to 22 in 2018).
The prospect of that trend persisting is a worry for prison officers. “We try our best, but if we got an influx [of older people], there’s no way we would be able to house them all safely,” Michael says.
His concerns may be justified. A 2018 report on social care in prisons by HM Inspectorate of Prisons and the Care Quality Commission found the prison service was failing to plan for the future needs of an increasingly elderly prison population. The MoJ says it has set out a programme of work to respond to the recommendations in the report.
Just months before, the HMPPS made a series of recommendations to help governors better meet the needs of older prisoners.
Among the suggestions in the toolkit are guidance on caring for prisoners with dementia, suitable amendments to regime, access to activities and additional end-of-life support. It is unclear, however, what progress has been made since implementing the guidance, says the Prison Reform Trust. The charity wants to see the guidance supported by mandatory requirements and progress monitoring.
Some prisons do appear to already have examples of good practice in place. HMP Leyhill and Eastwood Park have day centres run by the charity Recoop, while Stafford and Wymott have spaces designed for meaningful activities for older prisoners.
A prison officer, speaking to The Independent, talks about an older person’s tea club at the jail where he works: “Anyone over the age of 65 is invited to attend and they have tea, coffee and biscuits. It happens weekly.” He hints, though, that it is not always easy to ensure the meetups always go ahead. “Unfortunately, it comes down to resources,” he adds. “I don’t want to link back to 2010 but we lost almost 10,000 staff.”
Besides the physical obstacles across the estate, older prisoners are being supervised by staff who say they do not have adequate training for managing the often complex and multiple needs of older people. “We don’t get as much training on that; in terms of looking after the elderly, we’re not trained for that,” says Michael. “And there’s not enough people in the jail that are trained.”
William concurs and says there was nothing in his training that specifically enabled him to support older prisoners. Nevertheless, he believes this lack does not mean he is unable to be a compassionate prison officer. “The way I look at it is if one of my relatives, one of my friends were to end up in prison, how would I want them to be treated,” he says. “I always try to replicate that in the way I deal with people. Everyone is just one mistake away from being there, one mistake away from a custodial sentence.”
A Prison Service spokesperson said: “An ageing prison population poses particular challenges, which is why we work closely with local councils and healthcare providers to best meet the needs of those inmates. All governors have been sent guidance and best practice examples on how to care for older prisoners, and inspectors have praised initiatives such as other offenders supporting the elderly through a buddy scheme.