Home
- Janey Antoniou award (2019)
- Group of the year award (2023)
- University of Lancashire team award (2025)
1. Janey Antoniou Award 2019
Meet Sue Wheatcroft, winner of the 2019 Janey Antoniou Award.
09 November 2019
Today, Saturday 9 October, we are pleased to announce Sue Wheatcroft as the winner of our 2019 Janey Antoniou award for 2019. Sue is a campaigner and group coordinator who lives with Borderline Personality Disorder (BPD). She has made a huge difference on both a local and national level and the judges felt she exemplified what the Janey award is about – challenging stigma and creating change for people living with mental illness. We sat down with Sue to ask her more about her vital work.
What has your experience of the mental health system been like?
When I was in crisis, I asked my GP if I could increase my anti-depressants. He said I was already on the maximum dose and should think about talking therapy. I was referred to Talking Mental Health (IAPT), who said they couldn’t help. They referred me to secondary care, who gave me an assessment. I was then referred to a psychiatrist, who said he would put me on a waiting list for a psychologist and a CPN. I saw the psychiatrist three times within the next twelve months and each time he assured me I was still on the list. Eventually, I phoned the CMHT myself and was informed that I was not, and never had been, on any waiting list. From then on, my mental health worsened, and I offended. I spent 18 months in prison, during which time my (disabled) partner was forced into a nursing home. When it was all over, my partner (now wife) went home together. We have just celebrated 34 years together. We re-mortgaged the house so that I could have private therapy and I am now in recovery.
How did you start campaigning on mental health?
There are currently no dedicated mental health services for personality disorders (PDs) in Derbyshire. This means that, if someone presents to their GP with a PD, they are often told that nothing can be done because ‘there is no PD pathway in Derbyshire’. If they are lucky enough to be referred to an IAPT, they are often turned away because of the stigma of their condition. If they make it to the allowed six sessions and it turns out that it is not suitable, they can be discharged from the whole service for ‘not engaging’. It is common for an individual to be told that they are too complex for a service, or not complex enough. Inevitably, they lose faith in the system. Self-harm and suicidal ideation are common. One in ten people with BPD end their own life and seven in ten make a serious attempt.
What led you to setting up the BPD support group?
When I left prison, I re-mortgaged my house to pay for private therapy. I have been seeing the therapist every week since (it will be three years in February). For some of that time, I received a Personal Health Budget. Even so, I have spent an enormous amount on therapy, but it has been worth every penny. Without it, I know I would not have been able to carry on. However, I realise that not everyone can afford it, and, in the absence of statutory services, there is absolutely no help for people with a PD. There are many PDs, but I only have experience of BPD. The thought of others going through the same experiences as me, makes me feel physically ill. I set up the support groups to help ensure this doesn’t happen.
What was one of your proudest moments when campaigning on mental health…
…was when I first read out my story ‘First Night’ at a conference on ‘Commissioning Together’, organised by Health and Justice and attended by Lord Bradley (author of the Bradley Report). The positive reaction it elicited made me realise how much could be achieved by sharing lived experience. The story was about the shock, guilt, vulnerability and sense of desperation I experienced on my first night in prison. I realised then that it was a way of getting the consequences of inadequate mental health services known to a wider audience than just my home county. This does not retract from the fact that I take ‘ownership’ of my offences.
My most memorable moment is 200 members of the Independent Prison Board singing happy birthday to me after I had given a speech about BPD at a conference in Telford.
My proudest moments relating to the BPD support groups occur every time I witness the support, they give to each other. This can be at a meeting or on the group’s WhatsApp page.
How would you like to see care for BPD change?
I believe that the majority of people, once they have come to terms with their diagnosis, realise that not much can be done for them when in crisis. Two solutions have been suggested by the members. The first is to have a safe place to where they can be taken, voluntarily, to calm down. This could be some kind of crisis centre offering a few hours, or perhaps one or two days, away from the environment in which they reached crisis point. Once there, and this is also the second solution, they should be able to speak to someone who understands; is not judgemental; and has compassion. BPD is highly stigmatised, and individuals are often being accused of attention-seeking, manipulative and acting like a child. This last point is particularly interesting as most would agree that they display childish tantrums. They don’t want to; they can’t help it and are usually ashamed and embarrassed afterwards. Some professionals believe that people with BPD retain the emotional age at which they suffered childhood trauma. Someone can have the mind, body and intellect of an adult but the emotions of, say, a seven-year-old.
Before reaching crisis, and as an attempt to avert it, it is vital that the stigma surrounding BPD, and other PDs, is addressed. I would like to see zero tolerance on derogatory language (attention-seeker, for example). This should be made clear when receiving education and training on personality disorders which, at the moment, is woefully inadequate. Such courses should be made available to all health and justice professionals. This would include psychiatrists and psychologists, as they are often the instigators of stigmatising behaviour. It should also include police, probation and prison officers. People with PDs often end up in the Criminal Justice System. Seventy per-cent of people in prison have a personality disorder. BPD is the most common PD among women in prison.
Derbyshire NHS Trust say they will put more money into talking therapies. This is useless to those with a PD if they are excluded from the service in the first place, or if it is unsuitable for them. This is why we need a pathway (most other counties have one). All training should include facilitators who have lived experience.
It is important that you are passionate about the cause for which you are campaigning. It will be hard work and the sense of responsibility can give you sleepless nights sometimes, but every success, however small, can give you the greatest feeling in the world.
Sue WheatcroftJaney Antoniou winner 2019
How did it feel to win the Janey award?
I received the email whilst at the Supreme Court, where I had given a speech on the stigma of BPD. I wanted to shout it out to everyone but someone else was speaking and I had to be quiet. Also, I knew I had to be careful who I told so that it wasn’t put on social media. I couldn’t wait to get home to tell my wife, Vicky. She talked about putting it in the local paper as soon as I had the award so that everyone will know. Once I had calmed down, I realised how it could help to raise the profile and awareness of BPD, not just in Derbyshire but nationally. I feel very proud but also grateful, to the voting panel, Rethink, the group members and the many organisations and individuals who have given me a chance to campaign.
What would you say to people who would like to start campaigning on mental health, but don’t know where to start?
It is important that you are passionate about the cause for which you are campaigning. It will be hard work and the sense of responsibility can give you sleepless nights sometimes, but every success, however small, can give you the greatest feeling in the world. On a practical level, Rethink Mental Illness is well-equipped to help with such things as the Constitution; Insurance; Code of Conduct; risk-assessment for the venue; DBS checks for co-ordinators; and the other seemingly tiresome but vitally important aspects of setting up a support group. They can also help with promotion, such as leaflet distribution, and will offer continuing support.
If you are unsure about taking such a large step straight away, have a look at the Rethink Mental Illness website for other groups you could attend to find out more about how it is done. Bear in mind that a niche group, such as BPD, will probably be a slow-burner and it’s important that you don’t get despondent. On the other hand, a general mental health support group could take off straight away and you must be prepared, so that you don’t get overwhelmed.
Janey Antoniou was a dear friend of Rethink Mental Illness and an inspirational colleague. During her 15 year career in mental health she worked tirelessly to improve the care of people living with mental health problems. Throughout all her achievements she lived with debilitating depression, anxiety and schizophrenia. The Janey Antoniou Awards recognise campaigners with lived experience who have made a difference to the lives of people living with mental illness through raising awareness, combating stigma and campaigning for better care.
2. Group of the Year Winner 2023
Meet Derbyshire BPD Support Group, our 2023 Group of the Year winner (rethink.org)

After coming out of a four-year crisis, Sue wished there was a specialised BPD support group she could have been a part of. She’d attended more general mental health groups before but didn’t feel these were focused enough on her diagnosis. She created the Derbyshire Borderline Personality Disorder group in 2017, with wishes that nobody else would have to go through what she went through. Sue believes that her mental health crisis was exacerbated by the lack of support.
By the time Covid-19 came around the group had established four venues, but these had to shut because of the pandemic. Instead, the group went online via Zoom. The use of Zoom enabled the group to hugely expand with over 350 users, 13 of which were overseas. The group develops and progresses organically to meet people’s different needs; for example, the group stayed online but smaller and more local in-person events were set up, such as coffee mornings and activities like bowling (funded by external givers).
The group encourages members to create their own networks and Sue hopes that the group is just the start of smaller networks that develop and grow within themselves. It also offers information about themselves, referral advice, what the statutory services can offer and a quarterly newsletter. This newsletter allows people to contribute and share their own stories, share creative work such as art and poetry, features advice articles and articles about famous people living with BPD, as well as any new information or research. The group also has crisis cards for its users, designed for instances when they may get picked up by the police, paramedics etc, to explain that this individual is in a crisis and is not a criminal. Sue has also set up an Attachment Group which is run via email. Attachment is a huge part of living with BPD so the group offers exercises on dealing with attachment.
As well as this, a key part of the development of the group has been creating WhatsApp groups for specific needs. Six of these WhatsApp groups have now been established:
- General group chat. This has around 100 members.
- Positivity group. Sue understands that with mental illness comes its negative reality. No negative text is allowed in this chat to give people a positive boost for their day.
- Men with BPD.
- Parents with BPD.
- Virtual Walking Group where people send in pictures of their walks, such as canals or woodland, to then encourage people to get out into the fresh air.
- Parent and Carer Group.
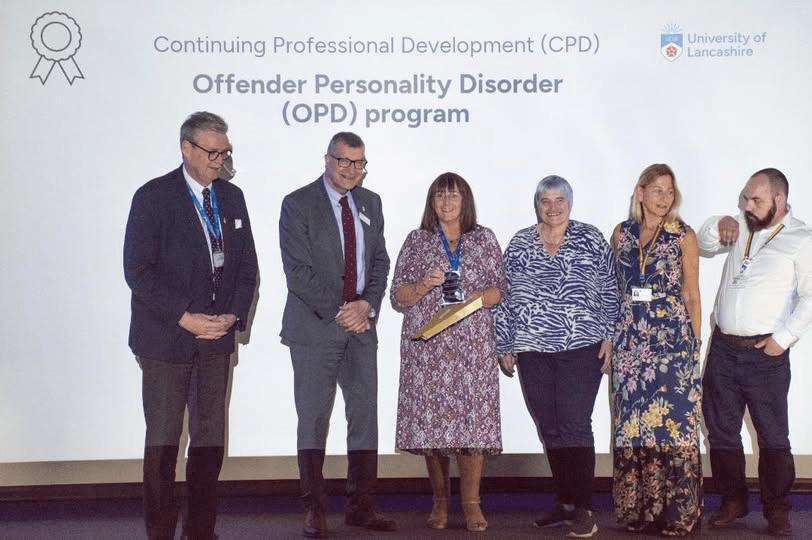
3. University of Lancashire team award (2025)